Diversity in academic hiring: a success story
CZ Biohub SF-backed NextGen initiative succeeds in diversifying faculty hiring in biological and biomedical sciences at major Bay Area universities
When the Chan Zuckerberg Biohub’s Paul Lebel first designed and built a microscope that uses ultraviolet (UV) light, he figured it would simply be a helpful research tool for scientists. Little did he imagine the scope would have a practical use as potential life-saving device.
But what started as an experimental new way of looking at cells and pathogens is now culminating in three prototype devices on their way to Uganda, to be field-tested as a potential way to more cheaply, accurately, and efficiently diagnose malaria.
For a disease with an annual burden of 241 million cases and over 600,000 deaths – primarily children in impoverished regions – a more efficient diagnostic is long overdue. Over the last century, public health workers have used a method called Giemsa staining to diagnose malaria. The method requires blood to be manually smeared onto a microscope glass slide, then treated chemically, then finally stained with a special formulation that gives the Plasmodium malaria parasites a bright color.
Skilled microscopists spend hours preparing samples before meticulously analyzing one at a time under the microscope, searching for the characteristic color and shape of malaria-causing parasites in blood cells. The method is time-consuming and prone to errors, even for the most experienced microscopists.
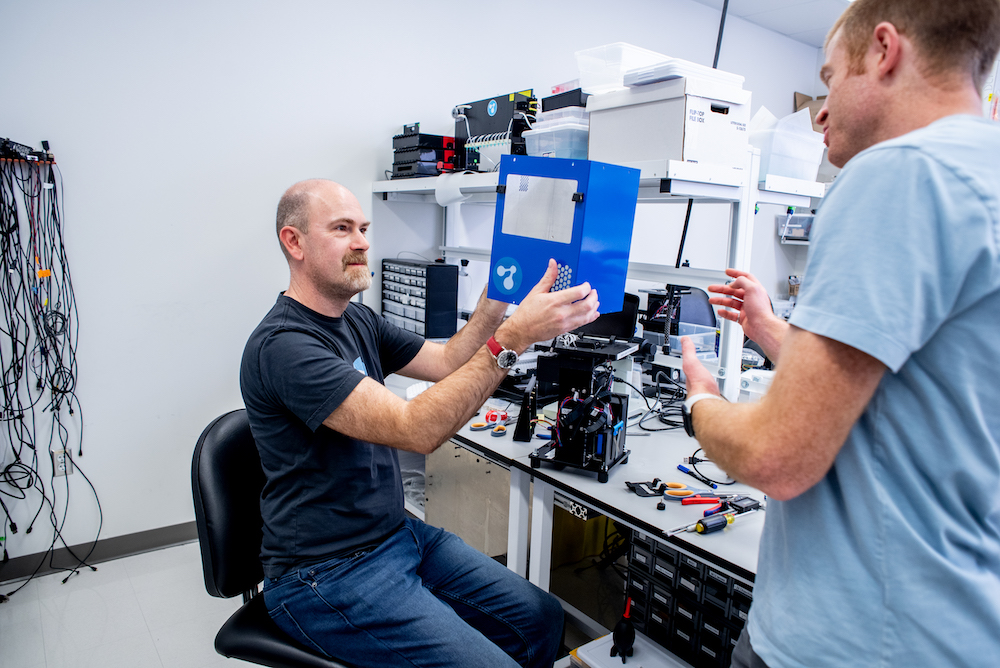
Biohub engineers Chris Charlton (left) and Paul Lebel prepare a new microscope for shipment to Uganda for field tests in Uganda. (Credit: Barb Ries)
“People who are trained in malaria microscopy might inspect 20 slides in one day, but that’s 12 hours of staring down the barrel of a microscope,” says Lebel, a CZ Biohub engineer in the Bioengineering team. “People get tired and they make mistakes.”
In recent years lateral-flow rapid diagnostic tests (RDTs) for malaria, similar to the rapid tests used today for COVID-19, have been broadly employed in the field due to their low cost. However, the malaria parasite can develop mutations that make these tests ineffective, and health workers in malaria-endemic regions often doubt their accuracy, as they can be counterfeited or produced with very low quality.
Another modern option for diagnosis is a PCR test, which detects the genetic material from Plasmodium parasites. PCR is much more accurate and sensitive than the Giemsa stain or lateral-flow tests, but it’s quite expensive and requires specialized lab equipment, making it impractical for widespread use in the lower-income regions of the world where malaria is prevalent.
Lebel’s new microscope was meant for examining things like viral protein clusters, structures within the nuclei of cells, and bacteria. “Then Joe DeRisi suggested we try looking at malaria parasites under the microscope,” he says.
DeRisi, president of CZ Biohub and an infectious disease expert, believed Lebel’s custom microscope could be the key to a more efficient diagnostic. To Lebel’s delight, when he and DeRisi examined malaria-infected blood under the UV microscope, they spotted the malaria parasites immediately – no antiquated slide staining technique required. “It was pretty compelling,” says Lebel.
Now, after many refinements of the microscope’s design, incorporating a built-in machine learning component, and testing its limits in the lab, the Bioengineering team has sent three custom-built automated UV microscopes to a clinic in Tororo, Uganda operated by colleagues from UC San Francisco. “Taking a one-off research tool and developing it into something robust, low-cost, and deployable has been a real team effort,” says Lebel. “This project could never have been accomplished without a stellar team of highly-motivated people. Chris Charlton, Emily Huynh, Ilakkiyan Jeyakumar, Michelle Khoo, Axel Jacobsen, and William Wu from the Bioengineering team, and Aditi Saxena from the DeRisi lab, have all contributed.”
The field tests will assess how well the microscope can do versus the Giemsa stain “gold standard,” as that remains the most trusted and widespread method used to diagnose the disease in the field.
The Biohub’s custom UV microscope aims to leverage the age-old effectiveness of microscopy while relieving the time-consuming labor component, improving consistency, and reducing the time from sample to result.
The microscope uses near-UV light with a wavelength that is highly absorbed by hemoglobin in red blood cells, but not by Plasmodium parasites. Therefore, when a malaria parasite is present in the cells, it shows up like a bright shape against a dark background. “The parasite looks bright, because it’s actually pushing away the hemoglobin around it,” Lebel explains.
Even more exciting, he says, was the fact that the researchers were able to visualize live parasites in fresh blood samples without having to dry, fix, or stain the samples.
A blood sample with lab-cultured malaria parasites, as captured by CZ Biohub’s malaria microscope. (Credit: CZ Biohub)
To further eliminate potential sources of error and cut down on time – and not have to rely on human observers – the researchers incorporated machine-learning algorithms that learn to detect the parasites automatically. The team published the design and results of their lab tests in PLOS Computational Biology in 2021, and are now putting their microscopes to the test in a real-life clinical setting.
By automating as much of the diagnostic process as possible, the team is aiming to produce a device that nearly anyone could use. The current iteration only requires the technician to dilute the blood sample before placing it in a little disposable cartridge, and then the microscope and its machine-learning capability does the rest. Eventually, “the goal is to even automate the dilution step within the device, so that dilution by hand is no longer required,” says Rafael Gómez-Sjöberg, leader of the Bioengineering team.
Not only will the microscope improve accuracy and decrease costs for malaria detection around the world, it will also significantly reduce the time it takes to get a diagnosis, which will help local healthcare providers determine the severity of an infection and choose a course of treatment.
“If a patient has a bad case of malaria, the device will tell you within 10 to 15 seconds that there’s a lot of Plasmodium present,” Lebel says. “You can get an answer almost as quickly as you can extract the blood from someone’s fingertip.” If a patient is either healthy or has a very low parasite burden, on the other hand, it could take up to 20 minutes for the device to provide a clear answer – but that is still quicker than the time it takes to prepare and analyze a Giemsa smear. Additionally, because smears are often prepared and analyzed in batches, it can take more than 24 hours for a patient to receive a diagnosis.
“Another very important application is being able to track the effectiveness of treatment by determining if the number of parasites is going down when people receive therapy,” says Gómez-Sjöberg. “Both RDTs and PCR give positive results even weeks after an infection has been cleared by treatment, so they can’t reveal in real time whether the number of parasites in the blood has changed in response to treatment, which is crucial for clinicians to know whether a given treatment is working or if they need to change drugs so the parasite doesn’t develop resistance. That’s a very important application of this device that has no equivalent.”
Additionally, knowing how prevalent the parasite is in the blood can help doctors diagnose if it’s malaria or some other pathogen that’s making a patient sick, Lebel says. In areas where malaria is endemic, many adults carry low levels of the parasite but are not symptomatic. If someone comes into a clinic sick from the flu or from typhoid fever and an RDT scores the patient as positive for malaria, they may be treated for malaria even though it might not be the cause of their illness. But if the doctor using the new scope saw there aren’t many malaria parasites present, they could decide to run other tests to determine the cause of illness.
The team is optimistic that the clinicians in Africa will need no more than a bit of training over Zoom to learn to run the microscopes. “A lot of the engineering effort we’ve put in is precisely to make the device easy to operate and as robust as possible,” Gómez-Sjöberg says.
The freedom to explore and to take the time to create such novel instruments without the pressure to publish quickly or win grants is “one of the secret sauces” that makes the CZ Biohub stand out from other research institutes, Lebel says. “Our mandate is to help scientists, so when a scientist like Joe comes up and says ‘Hey, let’s image malaria,’ we can say, ‘Yeah, let’s do this! Let’s build a new microscope!’”
CZ Biohub SF-backed NextGen initiative succeeds in diversifying faculty hiring in biological and biomedical sciences at major Bay Area universities
Learn More
CZ Biohub San Francisco Investigator Hawa Racine Thiam’s new Stanford lab applies physics to the study of cells and their nuclei
Learn More
A ‘Google Earth’ of embryology, CZ Biohub San Francisco's zebrafish cell atlas brings a new vision to developmental biology
Learn More
Stay up-to-date on the latest news, publications, competitions, and stories from CZ Biohub.
Marketing cookies are required to access this form.